The 2017 ASEAN guidelines on valvular regurgitation represent a significant step forward in standardizing the diagnosis and management of this prevalent cardiac condition within the Southeast Asian region. These guidelines provide healthcare professionals with a comprehensive framework to ensure optimal patient care based on the latest scientific evidence and regional considerations.
Understanding Valvular Regurgitation
Valvular regurgitation, also known as valve insufficiency or a leaky valve, occurs when a heart valve doesn’t close tightly, allowing blood to flow backward through the heart. This condition can affect any of the four heart valves:
- Tricuspid valve: Located between the right atrium and right ventricle.
- Pulmonary valve: Situated between the right ventricle and the pulmonary artery.
- Mitral valve: Positioned between the left atrium and left ventricle.
- Aortic valve: Lies between the left ventricle and the aorta.
Causes and Risk Factors
Various factors can contribute to valvular regurgitation, including:
- Congenital heart defects: Some individuals are born with malformed heart valves.
- Rheumatic heart disease: This condition, prevalent in developing countries, can damage heart valves.
- Infective endocarditis: Infection of the heart valves can lead to regurgitation.
- High blood pressure: Prolonged elevated blood pressure can strain the heart valves.
- Cardiomyopathy: Diseases affecting the heart muscle can impact valve function.
- Connective tissue disorders: Conditions like Marfan syndrome can weaken valve structures.
Symptoms of Valvular Regurgitation
The severity of symptoms can vary depending on the affected valve and the extent of leakage. Some individuals may remain asymptomatic for years, while others experience:
- Shortness of breath: Difficulty breathing, especially during exertion or lying down.
- Fatigue: Feeling tired and weak, even with minimal activity.
- Heart palpitations: Sensations of a rapid or irregular heartbeat.
- Swollen ankles, feet, or abdomen: Fluid retention due to heart inefficiency.
- Chest pain: Discomfort or pressure in the chest area.
 Common Symptoms of Valvular Regurgitation
Common Symptoms of Valvular Regurgitation
Diagnosis and Assessment
The ASEAN guidelines emphasize a comprehensive approach to diagnosing and assessing valvular regurgitation:
- Physical examination: Listening to the heart for murmurs and assessing for other clinical signs.
- Echocardiogram: This ultrasound scan provides detailed images of the heart’s structure and function, visualizing valve motion and blood flow.
- Electrocardiogram (ECG): Records the heart’s electrical activity and can detect rhythm abnormalities.
- Chest X-ray: Provides a view of the heart’s size and shape and can reveal lung congestion.
- Cardiac catheterization: This minimally invasive procedure measures pressures within the heart chambers and assesses valve function.
Management Strategies
Treatment for valvular regurgitation depends on the severity of the condition, the presence of symptoms, and the overall health of the patient. Options include:
- Medications: Drugs to manage symptoms like heart failure, arrhythmias, or high blood pressure.
- Lifestyle modifications: Adopting a heart-healthy diet, regular exercise, and quitting smoking.
- Valve repair or replacement surgery: This procedure aims to restore normal valve function, either by repairing the damaged valve or replacing it with a prosthetic valve.
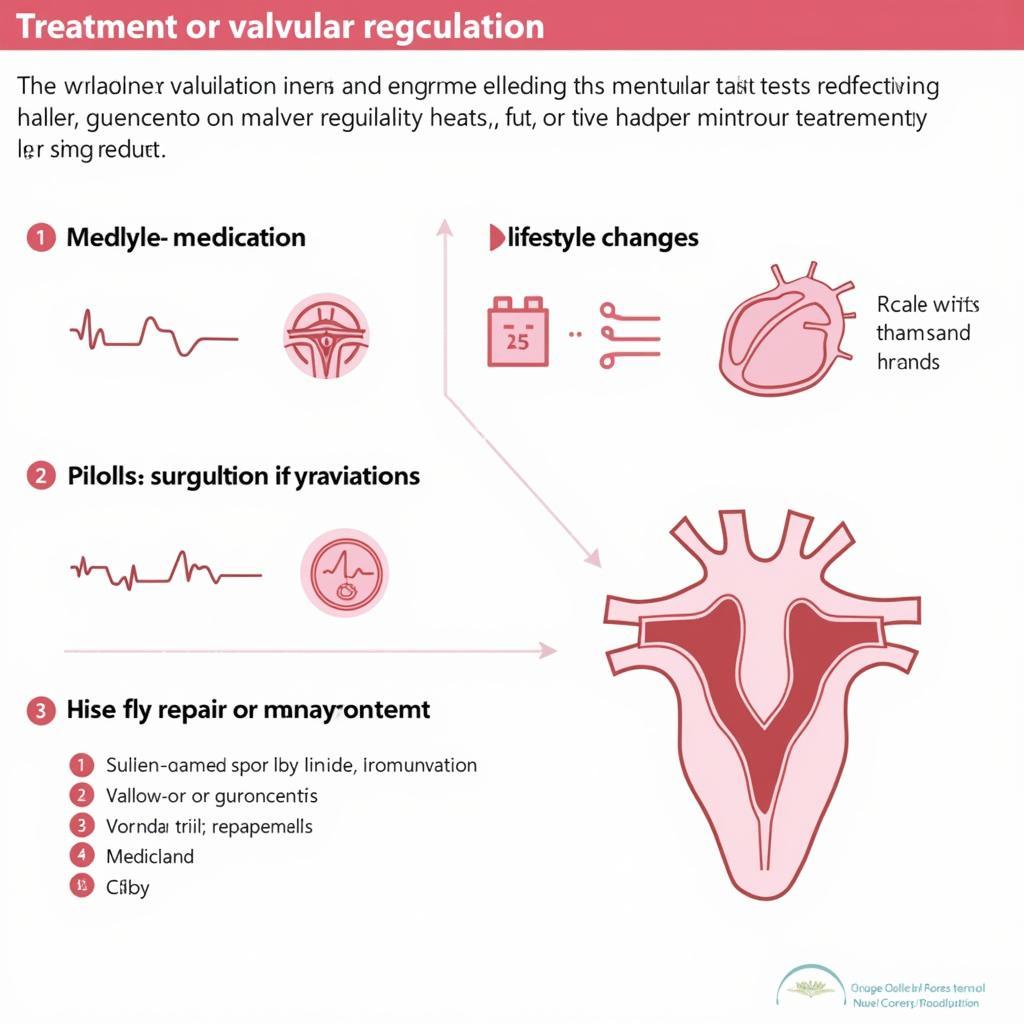 Treatment Options for Valvular Regurgitation
Treatment Options for Valvular Regurgitation
The Importance of Early Detection and Treatment
Timely diagnosis and appropriate management are crucial for improving outcomes in individuals with valvular regurgitation. Adhering to the ASEAN guidelines allows healthcare providers to:
- Identify individuals at risk: Early detection through regular check-ups and risk factor assessment.
- Initiate timely treatment: Prevent disease progression and minimize complications.
- Improve quality of life: Alleviate symptoms and enhance overall well-being.
Conclusion
The 2017 ASEAN guidelines on valvular regurgitation provide a valuable resource for healthcare professionals across Southeast Asia. By adhering to these evidence-based recommendations, healthcare providers can ensure standardized, high-quality care for individuals affected by this cardiac condition. Early detection, prompt intervention, and ongoing monitoring are key to optimizing patient outcomes and improving lives.