The term “ASEAN guidelines diastolic function” refers to the recommendations set forth by the ASEAN Society of Echocardiography for evaluating diastolic function, a crucial aspect of heart health. These guidelines, developed by leading cardiologists and experts in Southeast Asia, provide a standardized approach to assess how well the heart’s ventricles relax and fill with blood between heartbeats. This evaluation is essential in diagnosing and managing various cardiovascular conditions, including heart failure with preserved ejection fraction (HFpEF), a condition where the heart pumps normally but struggles to relax and fill properly.
The Importance of Standardized Diastolic Function Assessment in ASEAN
Accurate and consistent assessment of diastolic function is paramount for effective diagnosis and management of heart conditions, especially in the diverse ASEAN region. The ASEAN guidelines provide a common framework for healthcare professionals across the region, ensuring uniformity in echocardiography practices and interpretation of results. This standardization is particularly important given the varying levels of healthcare infrastructure and expertise across different ASEAN countries.
 ASEAN Echocardiography Guidelines
ASEAN Echocardiography Guidelines
Key Aspects of the ASEAN Guidelines for Diastolic Function
The ASEAN guidelines for diastolic function utilize various echocardiographic parameters to comprehensively assess the different phases of diastole, the period of ventricular relaxation and filling. These parameters include:
- Early Diastolic Mitral Inflow (E): Measured using pulsed-wave Doppler, this parameter reflects the early filling velocity of the left ventricle.
- Early Diastolic Annular Velocity (e’): Measured using tissue Doppler imaging, this parameter indicates the early diastolic relaxation velocity of the left ventricle.
- E/e’ Ratio: The ratio of E to e’ provides an estimation of left ventricular filling pressure, a key indicator of diastolic dysfunction.
- Left Atrial Volume: Measured using two-dimensional echocardiography, an enlarged left atrium can suggest chronic diastolic dysfunction.
- Tricuspid Regurgitation Velocity: This parameter, measured using continuous-wave Doppler, can indirectly assess pulmonary artery pressure, which is often elevated in individuals with diastolic dysfunction.
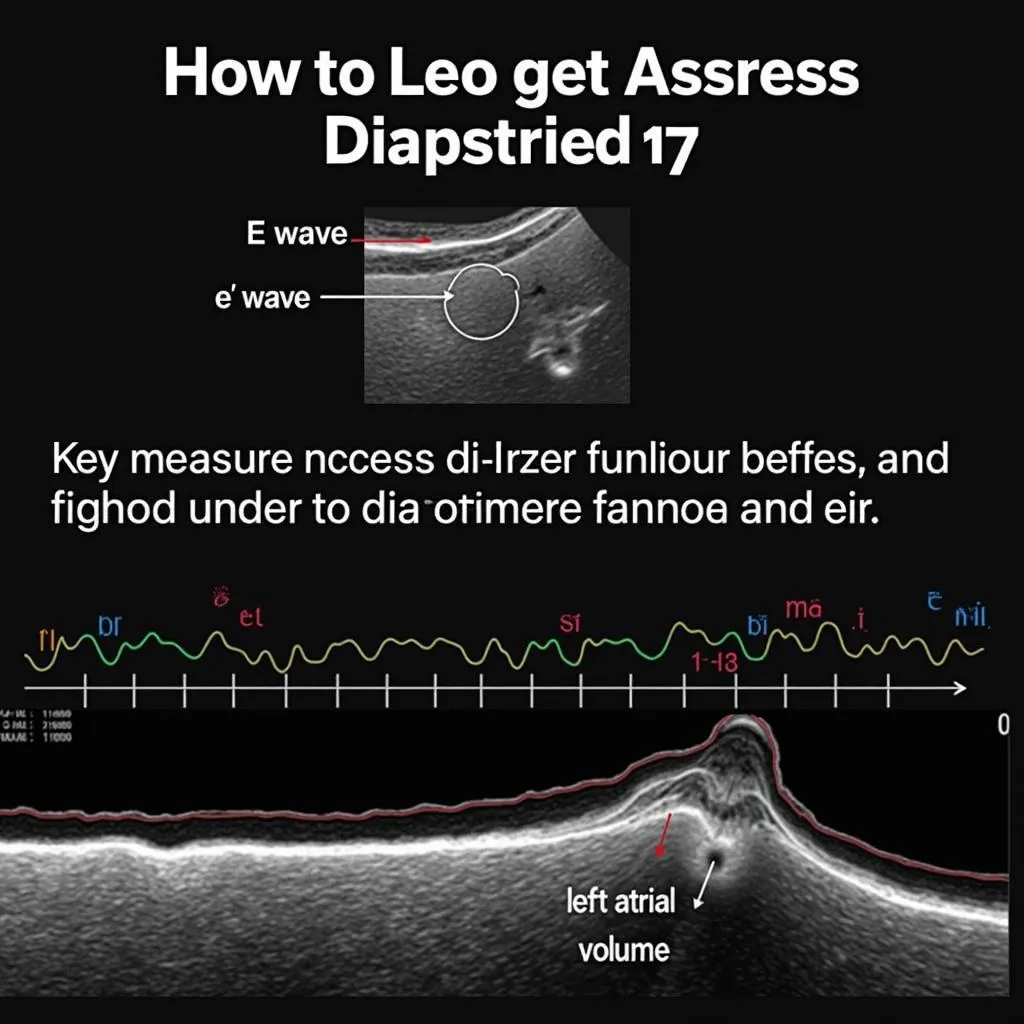 Echocardiogram with Diastolic Function Parameters
Echocardiogram with Diastolic Function Parameters
Implications of the ASEAN Guidelines for Patient Care
The standardized approach outlined in the ASEAN guidelines for diastolic function has significant implications for patient care in the region.
- Early Diagnosis: The guidelines facilitate early detection of subtle diastolic dysfunction, enabling timely intervention and potentially preventing progression to heart failure.
- Improved Management: Standardized assessment allows for more precise risk stratification and personalized treatment plans for patients with diastolic dysfunction.
- Enhanced Research: The uniform guidelines promote collaborative research efforts within ASEAN, leading to a better understanding and management of diastolic heart failure in the region.
Challenges and Future Directions
While the ASEAN guidelines for diastolic function represent a significant step forward, challenges remain in their implementation and widespread adoption.
- Training and Education: Continuous medical education and training programs are crucial to ensure healthcare professionals across ASEAN are proficient in applying the guidelines.
- Resource Availability: Equitable access to echocardiography equipment and trained personnel remains a challenge in some areas within the region.
- Ongoing Research: Continued research is necessary to refine the guidelines and adapt them to the evolving understanding of diastolic function and heart failure.
Conclusion
The ASEAN guidelines for diastolic function provide a vital framework for standardized assessment of this crucial aspect of heart health. By promoting uniformity in echocardiography practices and interpretation, these guidelines have the potential to improve the diagnosis, management, and ultimately, the lives of individuals with diastolic dysfunction across Southeast Asia. Continued efforts in education, resource allocation, and research will be key to fully realizing the benefits of these guidelines for the ASEAN community.


